Chronic Pain: What If Chronic Pain Becomes Too Much
For many individuals chronic pain is more than just a physical sensation it becomes a pervasive force that effects nearly every aspect of daily life. This persistent nature of chronic pain causes emotional distress, mental exhaustion, and an overwhelming sense of frustration. Over time, individuals may experience a decline in their overall quality of daily life, struggling with activities that once felt effortless. Simple tasks like walking, sitting, or even getting out of bed can become excruciating challenges, leading to a cycle of inactivity and aggravating pain.
Table of Contents
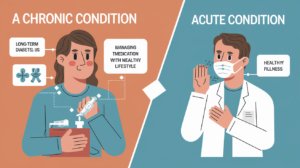
What is chronic pain?
Chronic pain is continuous pain that lasts for more than 3 to 6 months, often continuing beyond the initial injury and affecting daily routine. Unlike acute pain, which serves as a warning signal for injury and subsides with recovery, chronic pain stay beyond its expected healing time, sometimes without a clear cause. It can range from mild discomfort to severe, debilitating agony, affecting people in vastly different ways.
What if chronic pain is too much?
For many individuals chronic pain is more than just a physical sensation it becomes a pervasive force that effects nearly every aspect of daily life. This persistent nature of chronic pain causes emotional distress, mental exhaustion, and an overwhelming sense of frustration. Over time, individuals may experience a decline in their overall quality of daily life, struggling with activities that once felt effortless. Simple tasks like walking, sitting, or even getting out of bed can become excruciating challenges, leading to a cycle of inactivity and aggravating pain.
Common signs and symptoms
Chronic pain symptoms vary from person to person. But the defining characteristic of chronic pain is that it lasts for more than three months. You may describe the pain as:
Aching
Burning
Shooting
Squeezing
Stiffness
Stinging
Throbbing
Symptoms and Causes What does chronic pain feel like?
Chronic pain signs and symptoms often present as unstoppable pain that can be dull, sharp, burning, or throbbing. It may aggravate with time and recur on and off. Pain often interferes with many aspects of life, affecting mobility, sleep, and emotional health. Insomnia worsens pain and sleep becomes trickier.
What causes chronic pain?
Several factors can cause pain to persist long after an initial injury or illness. Chronic pain includes various triggers, such as:
Tissue damage From injuries like a sprained ankle or surgeries.
Inflammation Conditions like arthritis may cause ongoing discomfort.
Nerve dysfunction The central neurological system may become overly sensitive to pain indicators.
Psychological factors Anxiety and stress can trigger pain perception.
Why Chronic Pain Can Come and Go Over Time
Chronic pain is uncertain and can come and go over time due to various factors, including underlying health conditions, stress levels, lifestyle habits, and even changes in the weather. Some days, the pain may feel more provoked, while on others, it may lessen, offering temporary relief. Fluctuations in pain can be influenced by physical activity, diet, sleep patterns, and emotional well-being. In addition, certain prolonged conditions, such as fibromyalgia or inflammatory disease, tend to have flare-ups followed by periods of lesser discomfort. Understanding these patterns can help individuals manage their pain more effectively by distinguishing triggers and adopting scheme to minimize their impact.
Common Types of Chronic Pain
Chronic pain can appear in various ways and affect different parts of the body. While its causes and severity vary from person to person.
Neuropathic Pain
It occurs when there is damage, dysfunction, or irritation of the nerves, leading to abnormal pain signals being sent to the brain. Unlike pain caused by injury or inflammation, nerve pain arises from tissues within the nervous system itself. It often feels like burning, shooting, tingling, or electric shock-like sensations.
Common causes of neuropathic pain include
Trigeminal neuralgia A condition causing severe, stabbing pain in the face due to irritation of the trigeminal nerve.
Diabetic neuropathy Nerve damage from high blood sugar levels, often leading to pain and numbness in the feet and hands.
Postherpetic neuralgia Persistent nerve pain following a shingles infection.
Sciatica Pain radiating down the leg due to compression of the sciatic nerve.
Treatment
It is often difficult to manage with traditional painkillers, and treatment may involve nerve-specific medications, physical therapy, or nerve stimulation therapies.
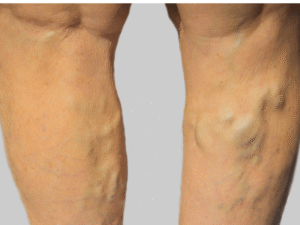
Musculoskeletal Pain
This pain affects the bones, muscles, joints, ligaments, and tendons. It can result from injury, wear and tear over time, or underlying conditions that cause chronic inflammation and discomfort. This type of pain may be localized or widespread, causing stiffness, aching, or sharp discomfort during movement.
Common causes of musculoskeletal pain include:
Fibromyalgia A condition characterized by widespread muscle pain, fatigue, and tenderness in specific areas of the body.
Chronic lower back pain Often caused by conditions like herniated discs, degenerative disc disease, or spinal stenosis.
Arthritis Inflammatory or degenerative joint conditions that lead to chronic pain and stiffness.
Tendinitis Inflammation of tendons, commonly affecting areas like the shoulders, elbows, or knees.
Treatment
Treatment for musculoskeletal pain could include physical therapy, stretching exercises, anti-inflammatory medications, and lifestyle modifications to reduce strain on affected areas.
Inflammatory Pain
It occurs when the body’s immune system responds to an injury or illness by triggering inflammation. This type of pain is often seen in autoimmune diseases, where the immune system mistakenly attacks healthy tissues, leading to persistent swelling, redness, and discomfort.
Common causes of this pain include:
Rheumatoid arthritis A chronic autoimmune condition that causes painful inflammation in the joints.
Lupus A systemic autoimmune disease that can cause widespread inflammation, affecting the skin, joints, and organs.
Inflammatory bowel diseases (IBD) Conditions like Crohn’s disease and ulcerative colitis that lead to chronic inflammation in the digestive tract, resulting in pain and discomfort.
Gout A form of arthritis caused by excess uric acid, leading to painful joint inflammation, particularly in the toes.
Treatment
Managing this type of irritative pain typically involves medications such as corticosteroids, disease-modifying anti-rheumatic drugs (DMARDs), and lifestyle changes, including anti-inflammatory diets and stress reduction techniques.
Chronic Visceral Pain
Visceral pain originates from the internal organs, such as the stomach, intestines, bladder, or reproductive organs. Unlike musculoskeletal or nerve pain, visceral pain is often described as deep, cramping, aching, or squeezing. It can be difficult to pinpoint because it may radiate to different areas of the body.
Common causes of chronic visceral pain include:
Irritable bowel syndrome (IBS) A disorder affecting the intestines, leading to chronic abdominal pain, bloating, and digestive issues.
Endometriosis A condition where tissue similar to the uterine lining grows outside the uterus, causing severe pelvic pain.
Interstitial cystitis A chronic bladder condition that leads to persistent pelvic pain and discomfort during urination.
Chronic pancreatitis Long-term inflammation of the pancreas, leading to severe abdominal pain.
Treatment
Because visceral pain can be difficult to diagnose, treatment often involves a combination of medication, dietary changes, and therapies aimed at managing symptoms and improving well-being.
Psychogenic Pain
It is also known as somatic symptom disorder, which refers to pain that has no clear physical cause but is influenced by psychological factors such as stress, anxiety, depression, or past trauma. While this type of pain does not stem from direct tissue damage, it is still very real and can be just as debilitating as other forms of chronic pain.
Common characteristics of this pain include:
Chronic headaches or migraines that intensify with stress.
Widespread muscle or joint pain with no identifiable medical cause.
Persistent back pain despite normal imaging results.
Pain that fluctuates with emotional distress or mood changes.
Treatment
Because this type of pain is closely linked to mental health, treatment often includes psychological therapy, stress management techniques, medication, and holistic approaches like mindfulness and relaxation exercises.
What are the risk factors for chronic pain?
Certain factors, such as aging, past injuries, and stress, can increase the risk for developing chronic pain, making early management essential, such as:
Age Older adults are at higher risk for conditions like back pain and rheumatoid arthritis.
Previous injuries Severe pain following an injury can become chronic.
Genetics Some individuals may have a predisposition to chronic pain syndrome.
Mental health disorders Anxiety and depression often exacerbate chronic pain.
Long-term use of pain relievers Dependency on commonly prescribed medications can lead to aggravated symptoms.
Pain syndrome A collection of symptoms that contribute to chronic pain.
Presence of pain The perception of pain even when no clear cause is present.
Insomnia aggravates pain Sleep is crucial for the body’s ability to heal and recover, but for those with chronic pain, getting restful sleep can be a challenge. Insomnia aggravate pain by preventing the body from repairing tissues and reducing inflammation. The lack of sleep also heightens pain sensitivity, creating a vicious cycle where pain disrupts sleep, and poor sleep further intensifies discomfort.
Diagnosis and Tests
How is chronic pain diagnosed?
A healthcare provider will perform a comprehensive evaluation, which might include:
Medical history To understand how long the chronic pain lasts and its impact on daily life.
Physical exams Identifying areas sensitive to pain.
Imaging tests X-rays, MRIs, or CT scans to identify tissue injury or nerve issues.
Nerve function tests Assessing neuralgia and nervous system involvement.
Signs and symptoms Evaluating how pain presents and affects daily function.
Management and Treatment That Improves Quality of Life
Chronic pain management requires a tailored approach. Effective Treatment options include:
Pain medication Including NSAIDs, opioids, and nerve painkillers.
Physical therapy Helps improve mobility and strength, particularly for musculoskeletal pain.
Pain management specialist A professional who develops personalized pain management plans.
Cognitive-behavioral therapy relieving pain through psychological techniques.
Steroid injections Blocking pain indicators in the central nervous system.
Alternative treatments acupuncture, massage, and XR Health’s virtual reality pain management.
Dampeners to pain Methods used to reduce pain sensitivity and perception.
Block pain signals Techniques used to disrupt pain pathways to block pain signals.
Therapies and lifestyle changes A combination of strategies to dampeners to pain and improve well-being.
If not managed properly, chronic pain deteriorate over time, creating a recurrent pattern of discomfort and distress. The consequences of pain can extend beyond physical symptoms, leading to severe chronic pain and mental health struggles.
Does chronic pain ever go away?
Chronic pain lasts indefinitely for some, but with the effective solution, it may be reduced. Managing pain effectively requires lifestyle changes, therapies, and medical interventions. It’s important to seek early intervention to prevent further complications. The right approach may involve trial and error, but it’s worth undertaking to find relief.
Outlook / Prognosis What is the prognosis (outlook) for people with chronic pain?
Chronic pain is too much to endure for many, affecting daily activities, emotional well-being, and overall general health. Chronic suffering can result to feelings of helplessness and diminished well-being. However, research shows that with proper pain management, many people experience significant relief. A pain management doctor can help manage symptoms and improve daily function.
What are the complications of this condition?
If left untreated, chronic pain can lead to:
Emotional distress Suicidal thoughts and suicide attempts may occur in extreme cases.
Reduced mobility Physical limitations that aggravate over time.
Medication dependency Long-term use of pain medication can have serious side effects.
Impact on relationships and work Chronic suffering could lead to social withdrawal and financial strain.
Creates a vicious cycle pain and stress reinforcing each other, making the condition harder to manage.
Pain can lead to secondary health problems, including cardiovascular issues.
Living With Pain Symptoms
You should seek help for chronic pain if:
Your chronic pain conditions are unmanageable and interfere with daily activities.
Pain that comes and goes becomes more severe.
Your pain worsens despite medication and treatment efforts.
You experience symptoms of depression or suicidal thoughts.
You are ready to find relief and need expert guidance.
You have experienced chronic pain for longer than expected and need a pain management plan.
There’s extra pressure on your joints or muscles that increases pain.
What questions should I ask my healthcare provider?
When visiting a healthcare provider, consider asking:
What is causing my chronic pain?
What management strategies are worth pursuing?
What are the best therapies and lifestyle changes for me?
What should occur if my chronic pain illness worsens?
What are the consequences of pain on my nervous system?
Are there alternatives to long-term pain meds?
How can I manage inflammatory pain and neuropathic pain effectively?
What are my options if standard treatment doesn’t work?
How does the central nervous system contribute to my pain?
How to make a diagnosis or treatment?
How to contact with pain management specialist?
Conclusion
One approach to effectively managing chronic pain is integrating medical treatments with lifestyle adjustments to enhance overall well-being and quality of life. Living with chronic pain is challenging, but managing pain effectively is possible. If chronic pain becomes too much, consulting a pain management doctor can provide relief. XR Health and other innovative approaches can help break the cycle of unrelenting pain. With the right approach, it’s possible to regain control and improve the standard of living. The time to find the right treatment is now, as pain should occur only as a temporary response, not as a long-term burden. Recovery from chronic pain may take time, requiring a combination of medical care, lifestyle changes, and therapy.