Chronic Metatarsalgia
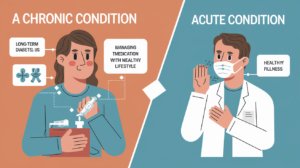
Chronic metatarsalgia is a condition that causes lasting or recurring pain in the ball of your foot, right behind your toes. This area, called the forefoot, supports your body weight when you walk, run, or stand. When the pressure here becomes too great or unbalanced, it can lead to irritation, pain, and inflammation. The discomfort can feel sharp, burning, or aching, and often worsens with activity.
Table of Contents
What Is Metatarsalgia?
Metatarsalgia is the medical term for pain and inflammation in the front of your foot. This pain usually centers under the metatarsal bones—the long bones that connect your ankle to your toes. It’s often felt under the second, third, or fourth toes and can affect one or both feet.
Common triggers include:
Structural foot problems like high arches or bunions
Medical issues like arthritis or nerve conditions
Impact-heavy activities like running or sports
Wearing unsupportive or tight footwear
Initial treatment usually involves rest, better footwear, and pain relief techniques.
Symptoms and Causes
Symptoms of Metatarsalgia:
Persistent pain or aching in the ball of the foot
Sharp or burning sensations during movement
Tingling or numbness in the toes
Feeling like there’s a pebble inside your shoe
Increased pain with standing, walking, or running
What Causes It?
Metatarsalgia is often caused by too much pressure on the forefoot. This can result from several factors:
Structural or primary causes:
High foot arches or flat feet
Bunions or hammertoes
Second toe being longer than the big toe
Thick calluses under the forefoot
Secondary causes (health and activity):
Arthritis (especially rheumatoid), gout, or Morton’s neuroma
Diabetes and obesity
Long-distance running, jumping, or similar sports
Worn-out shoes or walking barefoot often
Post-surgical or iatrogenic causes:
Changes in foot alignment after bunion surgery
Improper healing from fractures
Loss of bone tissue due to poor blood flow (avascular necrosis)
Who Is at Risk?
While anyone can develop metatarsalgia, you’re more at risk if you:
Are active in high-impact sports
Wear high heels or shoes with little cushioning
Are overweight or obese
Have existing foot deformities
Have conditions like diabetes or nerve disorders
Possible Complications
If left untreated, chronic metatarsalgia can lead to:
Continued pain and discomfort
Changes in your walking pattern
Stress on knees, hips, or back
Increased risk of stress fractures
Diagnosis and Testing
Doctors usually diagnose metatarsalgia through:
A physical foot exam
Questions about your symptoms and activities
Imaging like X-rays to rule out fractures
MRI or ultrasound to check soft tissues and nerves
Treatment Options
Most cases improve with conservative care:
Rest and Ice: Let your foot heal and apply ice to reduce swelling
Pain Relief: Use OTC medications like ibuprofen or acetaminophen
Proper Footwear: Switch to supportive, well-cushioned shoes with room for your toes
Inserts and Padding: Use metatarsal pads or orthotic insoles to redistribute pressure
Stretching and Strengthening: Gentle foot and ankle stretches, guided by a physiotherapist
If your pain continues, more advanced care may include:
Cortisone injections for inflammation
Physical therapy to correct foot mechanics and build strength
Surgery in rare cases to fix deformities or release nerve pressure
Prognosis
With the right care, most people recover well from metatarsalgia. You may feel better in a few weeks once pressure is relieved and inflammation goes down. Chronic or untreated cases may take longer and require professional care.
How to Prevent Metatarsalgia
You can lower your risk by:
Wearing shoes with cushioned soles and wide toe boxes
Avoiding high heels or narrow, tight shoes
Using shoe inserts for support
Keeping your feet clean and callus-free
Maintaining a healthy body weight
Living With Metatarsalgia
See a doctor if:
Your symptoms last longer than two weeks
Pain stops you from normal activity
You feel numbness, tingling, or swelling
You have diabetes and any foot pain
Ask Your Doctor:
What caused my foot pain?
Do I need X-rays or other tests?
What shoes or inserts should I use?
When can I return to physical activity?
Can this condition come back?
Final Thoughts
Living with chronic metatarsalgia can be frustrating, especially when foot pain limits your daily movement. But with the right steps—like wearing proper shoes, using padding, doing gentle stretches, and seeing a professional when needed—you can manage symptoms and protect your feet long term. Listen to your body, don’t ignore persistent pain, and take early action to prevent future complications.