Amenorrhea Symptoms Causes Treatment
amenorrhea symptoms causes treatment is topic that we are going to discuss with amenorrhea diagnosis and icd 10. Amenorrhea, the absence of menstrual periods in women of reproductive age, is a complex and multifaceted medical condition. It can have profound physical and emotional effects, impacting a woman’s overall health and wellbeing. In this comprehensive article, we will delve into the various aspects of amenorrhea, exploring its definition, symptoms, diagnostic criteria, causes, treatment options, surgical interventions (if applicable), rehabilitation, and management strategies.
Definition and ICD10 Code for Amenorrhea
Amenorrhea is defined as the absence of menstrual periods for three or more consecutive menstrual cycles in women of reproductive age. In the International Classification of Diseases, Tenth Edition (ICD10), it is classified under codes N91.0 for primary amenorrhea and N91.1 for secondary amenorrhea. These codes assist in medical recordkeeping and billing, ensuring standardized healthcare data.
Symptoms of Amenorrhea
The most apparent symptom of amenorrhea is the absence of menstrual periods. However, it is essential to recognize that amenorrhea itself is not a condition but rather a symptom of an underlying issue. Women with amenorrhea may experience symptoms related to the underlying cause, which can include hormonal imbalances, changes in mood, hot flashes, night sweats, vaginal dryness, and infertility. Additionally, the emotional and psychological impact of amenorrhea, particularly in those desiring to conceive, can be significant.
Causes and Risk Factors
Amenorrhea can have various underlying causes, including hormonal imbalances (e.g., polycystic ovary syndrome, hypothalamic dysfunction), structural abnormalities (e.g., congenital anomalies), medications, stress, excessive exercise, and significant weight loss or gain. Risk factors for amenorrhea may include family history, intense athletic training, eating disorders, and certain medical conditions. Identifying and addressing the root cause is crucial for effective management.

Diagnostic Criteria and Tools
The diagnosis of amenorrhea involves a thorough evaluation of a woman’s medical history, a physical examination, and often a series of tests. Diagnostic tools may include blood tests to assess hormone levels (e.g., FSH, LH, estradiol, thyroid function), imaging studies (e.g., ultrasound, MRI), and potentially a pelvic examination. The diagnosis distinguishes between primary and secondary amenorrhea and aims to identify the underlying cause.
Epidemiology of Amenorrhea
The prevalence of amenorrhea varies depending on the underlying causes. For example, primary amenorrhea is less common than secondary amenorrhea. Conditions like polycystic ovary syndrome (PCOS) and hypothalamic amenorrhea can affect a significant portion of the female population. The epidemiology of amenorrhea is influenced by factors such as age, genetics, lifestyle, and geographic location.
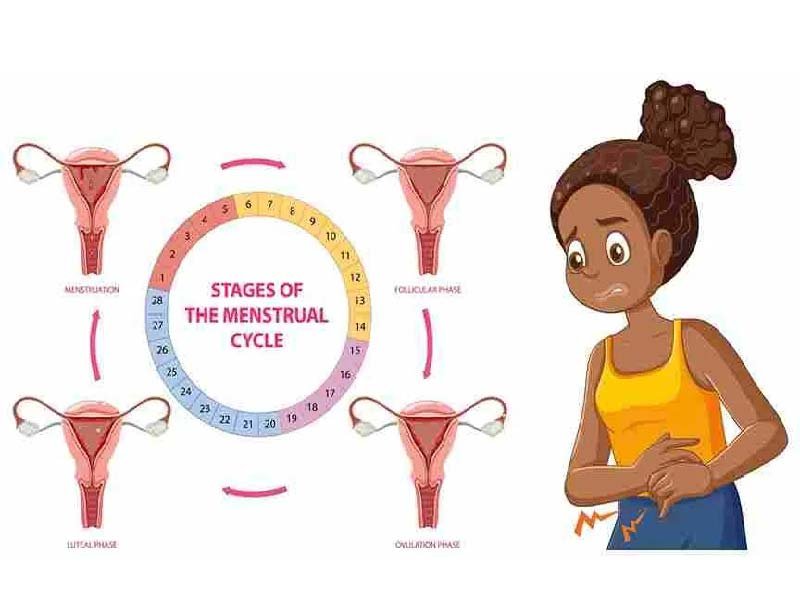
Pathophysiology
Amenorrhea can result from disruptions in the complex hormonal balance that governs the menstrual cycle. Primary amenorrhea often arises from congenital anomalies in the reproductive system, while secondary amenorrhea is frequently associated with underlying conditions affecting the hypothalamus, pituitary gland, ovaries, or uterus. Hormonal imbalances, such as elevated prolactin levels or thyroid dysfunction, can also contribute to amenorrhea. The pathophysiology varies depending on the underlying cause, but it usually involves the disruption of key reproductive hormones, including estrogen, progesterone, folliclestimulating hormone (FSH), and luteinizing hormone (LH).
Treatment Options for Amenorrhea
Treatment for amenorrhea depends on the underlying cause. In cases where lifestyle factors like excessive exercise or significant weight loss are at the root, addressing these issues can lead to the resumption of normal menstrual cycles. For hormonal imbalances, medication may be prescribed. For example, hormone replacement therapy (HRT) can help restore hormonal balance, while the use of medications like metformin may be beneficial in cases of PCOS.
Surgical Interventions (if applicable)
In some instances, surgical interventions may be necessary for treating amenorrhea. This is most common in cases of structural abnormalities such as uterine septum or cervical stenosis. Surgical correction of these anatomical issues can often resolve the amenorrhea and allow for normal menstrual function.
Rehabilitation and Management
Managing amenorrhea often involves lifestyle modifications and addressing the psychological aspects of the condition. This may include dietary changes, stress reduction, and psychological support. For women seeking to conceive, fertility treatments or assisted reproductive technologies may be necessary. Management strategies should be tailored to the individual, addressing both the physical and emotional aspects of the condition.
Conclusion
Amenorrhea is a symptom that can significantly impact a woman’s health and quality of life. Understanding the causes, symptoms, and available treatment options is crucial for both healthcare providers and affected individuals. Through appropriate diagnosis, treatment, and management, it is possible to address the underlying causes of amenorrhea and improve overall wellbeing. Research continues to shed light on this complex condition, offering hope for better management and outcomes in the future.